An Innovative Approach to Sepsis Prevention Saves Lives
Dec 6, 2013
Sepsis is a potentially deadly infection that causes your immune system to attack your body rather than protect it. It’s a leading cause of death in U.S. hospitals, accounting for five times as many deaths as heart disease.1 And while some survivors recover completely, others might experience long-term organ damage that harms their ability to live and work normally.
To mitigate the potentially deadly impact of sepsis, we developed a protocol that reduced sepsis-related deaths by 55% at our hospitals in Northern California. The treatment proved so effective that we’re sharing it with other hospitals and public health organizations. At the heart of the protocol: rapid, highly coordinated diagnosis and teamwork — something most other hospitals aren’t set up to deliver.
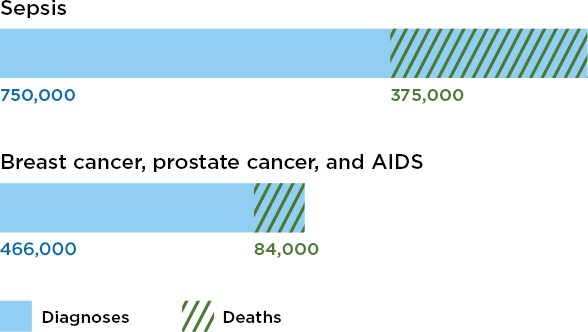
Annual impact of sepsis compared to other conditions
What makes sepsis hard to treat?
Because patients often develop sepsis before they get to the hospital, diagnosis and treatment during the initial “golden hour” timeframe becomes critical. Yet most hospitals struggle with this. In fact, only half of patients with septic shock — the most severe form — get effective treatment within six hours of onset.2 Here’s why:
- Sepsis is unpredictable. Sepsis occurs in all age ranges and can result from a variety of illnesses or injuries — even scraped knees.
- Symptoms are generic. The first signs of sepsis — fever, high pulse or breathing rate, elevated white blood count, nausea, and vomiting — are also symptoms of many other illnesses.
- Treatment is complex. Effective sepsis treatment requires swift collaboration among nurses, physicians, and specialists in different departments — and most hospitals aren’t structured to deliver this type of coordinated care.
Blazing the trail to better sepsis care
To make matters worse, a lack of published scientific evidence on the best way to treat sepsis meant there wasn’t a proven playbook for hospitals to follow. So in 2008 we formed our own sepsis mortality reduction team. Unlike physicians and hospitals that work independently of each other, our organizational structure, integrated electronic health record system, and team approach to care meant we could develop a set of best practices that would work across all of our hospitals. After working with quality and physician leaders to secure support for the initiative, the team recommended early, aggressive, and highly coordinated prevention and treatment as the keys to reducing sepsis-related deaths.
In Northern California, Kaiser Permanente’s Sepsis Mortality Reduction Initiative led to a dramatic increase in lives saved. The success of the program has impacted the entire organization.
Building a better playbook
Using an existing protocol called Early Goal-Directed Therapy as a starting point, the sepsis mortality reduction team launched pilot care programs at two of our Northern California hospitals. Care teams of intensive care specialists, rapid response nurses, pharmacists, physicians, and emergency department personnel were formed and given the task of designing a sepsis treatment playbook.
The care teams made improvements throughout the pilot period. Lab tests were consistently ordered earlier. Aggressive treatments were initiated according to specific vital sign ranges, clinical conditions, and timeframes. This gave physicians, specialists, and nurses the ability to adjust treatments not just within the critical “golden hour” window, but throughout the first six hours. And process metrics used to evaluate performance were developed. After initial success, the modified sepsis protocol was quickly expanded to other Kaiser Permanente hospitals in Northern California.
When diagnoses at our hospitals increased, deaths decreased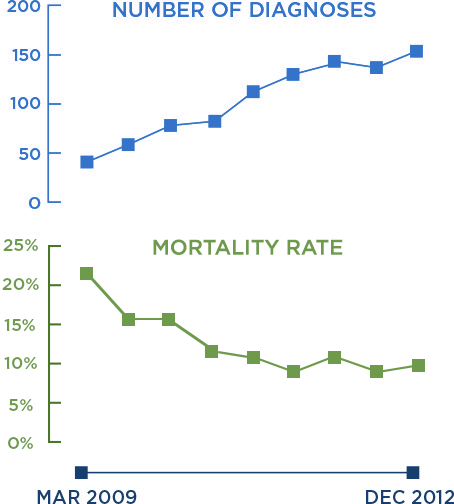
Highly effective results
Using the new playbook, the death rate from septic shock at participating California hospitals dropped from 21.2% to 9.5% (2009 to 2012).3 This is remarkable when compared to the national sepsis mortality rate of 28% up to 50%.4 And by January 2010, we decreased the length of hospital stays due to sepsis by 3.5 days.5 This represents significant savings — sepsis-related treatment incurs some of the highest hospital costs among diagnosed conditions.6
The sepsis in Northern California was so successful that it’s now in place at every Kaiser Permanente hospital. We also serve as a model for others — New York state looked to us for help on setting up a new, aggressive sepsis recognition and treatment program.7 And we’re working with the Joint Commission Center for Transforming Healthcare to create sepsis guidelines for all U.S. hospitals — with a goal of reducing sepsis deaths by 20% within 18 months. We’re also sharing our knowledge with the general public through tools like our free neonatal sepsis calculator.





DID YOU KNOW
— Heath and Heath, Decisive: How to Make Better Choices in Life and Work, 2013.